- 41 Pdf Previewdialectical Behavioral Training Certification
- 41 Pdf Previewdialectical Behavioral Training Techniques
Introduction
Dialectical behavior therapy (DBT) is a cognitive behavioral treatment that was originally developed to treat chronically suicidal individuals diagnosed with borderline personality disorder (BPD) and it is now recognized as the gold standard psychological treatment for this population. In addition, research has shown that it is effective in treating a wide range of other disorders such as substance dependence, depression, post-traumatic stress disorder (PTSD), and eating disorders. As such, DBT is a transdiagnostic, modular treatment.
The term “dialectical” means a synthesis or integration of opposites. The primary dialectic within DBT is between the seemingly opposite strategies of acceptance and change. For example, DBT therapists accept clients as they are while also acknowledging that they need to change to reach their goals. In addition, the skills and strategies taught in DBT are balanced in terms of acceptance and change. The four skills modules include two sets of acceptance-oriented skills (mindfulness and distress tolerance) and two sets of change-oriented skills (emotion regulation and interpersonal effectiveness).
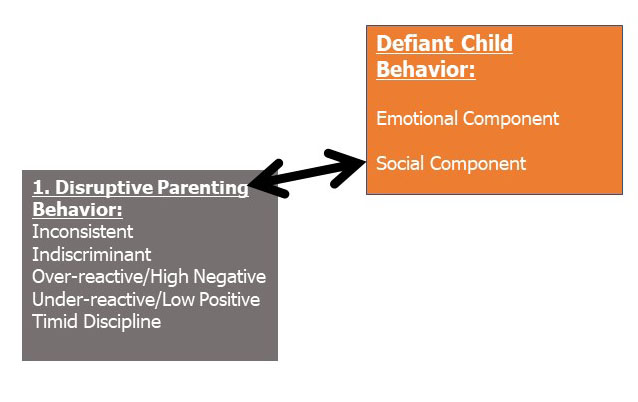
This document supersedes NIST SP 500-172, Computer Security Training Guidelines, published in 1989. The new document supports the Computer Security Act (Public Law 100-235) and OMB Circular A-130 Appendix III requirements that NIST develop and issue computer security training guidance. This publication presents a new conceptual framework for providing information technology (IT) security. Individual’s behavior is the result of two environmental stimuli: antecedents and consequences. Antecedents are stimuli or situations that signal that a behavior is expected, whereas conse-quences are stimuli that either strengthen the likelihood that the behavior will occur again or reduce the future occurrence of the behavior.
Components of DBT
- There are four components of comprehensive DBT: skills training group, individual treatment, DBT phone coaching, and consultation team.
- DBT skills training group is focused on enhancing clients’ capabilities by teaching them behavioral skills. The group is run like a class where the group leader teaches the skills and assigns homework for clients to practice using the skills in their everyday lives. Groups meet on a weekly basis for approximately 2.5 hours and it takes 24 weeks to get through the full skills curriculum, which is often repeated to create a 1-year program. Briefer schedules that teach only a subset of the skills have also been developed for specific populations and settings.
- DBT individual therapy is focused on enhancing client motivation and helping clients to apply the skills to specific challenges and events in their lives. In the standard DBT model, individual therapy takes place once a week for approximately 60 minutes and runs concurrently with skills groups.
- DBT phone coaching is focused on providing clients with in-the-moment coaching on how to use skills to effectively cope with difficult situations that arise in their everyday lives. Clients can call their individual therapist between sessions to receive coaching at the times when they need help the most.
- DBT therapist consultation team is intended to be therapy for the therapists and to support DBT providers in their work with people who often have severe, complex, difficult-to-treat disorders. The consultation team is designed to help therapists stay motivated and competent so they can provide the best treatment possible. Teams typically meet weekly and are composed of individual therapists and group leaders who share responsibility for each client’s care.
DBT Skills
DBT includes four behavioral skill modules, with two acceptance-oriented skills (mindfulness and distress tolerance) and two change-oriented skills (emotion regulation and interpersonal effectiveness).
- Mindfulness: the practice of being fully aware and present in this one moment
- Distress Tolerance: how to tolerate pain in difficult situations, not change it
- Interpersonal Effectiveness: how to ask for what you want and say no while maintaining self-respect and relationships with others
- Emotion Regulation: how to decrease vulnerability to painful emotions and change emotions that you want to change
There is increasing evidence that DBT skills training alone is a promising intervention for a wide variety of both clinical and nonclinical populations and across settings.
DBT Treatment Targets
Clients who receive DBT typically have multiple problems that require treatment. DBT uses a hierarchy of treatment targets to help the therapist determine the order in which problems should be addressed. The treatment targets in order of priority are:
- Life-threatening behaviors: First and foremost, behaviors that could lead to the client’s death are targeted, including suicide communications, suicidal ideation, and all forms of suicidal and non-suicidal self-injury.
- Therapy-interfering behaviors: This includes any behavior that interferes with the client receiving effective treatment. These behaviors can be on the part of the client and/or the therapist, such as coming late to sessions, cancelling appointments, and being non-collaborative in working towards treatment goals.
- Quality of life behaviors: This category includes any other type of behavior that interferes with clients having a reasonable quality of life, such as disorders, relationship problems, and financial or housing crises.
- Skills acquisition: This refers to the need for clients to learn new skillful behaviors to replace ineffective behaviors and help them achieve their goals.
DBT Treatment Stages
DBT is divided into four stages of treatment. Stages are defined by the severity of the client’s behaviors, and therapists work with their clients to reach the goals of each stage in their progress toward having a life that they experience as worth living.
41 Pdf Previewdialectical Behavioral Training Certification
- In Stage 1, the client is miserable and their behavior is out of control: they may be trying to kill themselves, self-harming, using drugs and alcohol, and/or engaging in other types of self-destructive behaviors. When clients first start DBT treatment, they often describe their experience as “being in hell.” The goal of Stage 1 is for the client to move from being out of control to achieving behavioral control.
- In Stage 2, they’re living a life of quiet desperation: their behavior is under control but they continue to suffer, often due to past trauma and invalidation. Their emotional experience is inhibited. The goal of Stage 2 is to help the client move from a state of quiet desperation to one of full emotional experiencing.
- In Stage 3, the challenge is to learn to live: to define life goals, build self-respect, and find peace and happiness. The goal is that the client leads a life of ordinary happiness and unhappiness.
For some people, a fourth stage is needed: finding a deeper meaning. Linehan has posited a Stage 4 specifically for clients for whom a life of ordinary happiness and unhappiness fails to meet a further goal of fulfillment or a sense of connectedness of a greater whole. In this stage, the goal of treatment is for the client to move from a sense of incompleteness towards a life that involves an ongoing capacity for experiences of joy and freedom.
DBT Research Findings
To date, there have been nine published randomized controlled trials and five controlled trials of DBT (view all publications). Two of these trials (carried out in our research clinic) specifically targeted highly suicidal women with BPD, and we are in the midst of a third trial targeting the same population. In our first study, results favoring DBT were found in each DBT target area. Compared to treatment-as-usual (TAU), DBT subjects were significantly less likely to attempt suicide or to self-injure, reported fewer intentional self-injury episodes at each assessment point, had less medically severe intentional self-injury episodes and lower treatment drop-out, tended to enter psychiatric units less often, had fewer inpatient psychiatric days, reported less anger, and improved more on scores of global as well as social adjustment. In our second study, we compared DBT to a much stronger control condition, treatment by non-behavioral community experts (TBE). In comparison to TBE, DBT reduced suicide attempts by half, had less medically severe self-injurious episodes, lower rates of treatment drop-out, and fewer admissions to both emergency departments and inpatient units due to suicidality. In studies of DBT for BPD patients that have been conducted outside of our research clinic, DBT has outperformed control treatments in reducing intentional self-injury, suicidal ideation, inpatient hospitalizations, hopelessness, depression, dissociation, anger, and impulsivity. In studies of substance dependent BPD patients conducted at our research clinic as well as at other sites, DBT has been found to be superior to control treatments in reducing substance use.
DBT Cost Effectiveness
Accumulating evidence indicates that DBT reduces the cost of treatment. For example, the American Psychiatric Association (1998) estimated that DBT decreased costs by 56% – when comparing the treatment year with the year prior to treatment – in a community-based program. In particular, reductions were evident by decreased face-to-face emergency services contact (80%), hospital days (77%), partial hospitalizations (76%), and crises bed days (56%). The decrease in hospital costs (~$26,000 per client) far outweighed the outpatient services cost increase (~$6,500 per client).

The cost effectiveness of DBT also extends past the treatment year as evidenced by a recent examination in a VA hospital setting. Meyers and colleagues (2014) found that veterans who received DBT treatment had significantly decreased the use of outpatient mental health services in the following year by 48%. Perhaps more importantly, the study demonstrated that utilization of high-cost inpatient services decreased by 50% and length of stay by 69%. The authors concluded that each individual in DBT treatment utilized almost $6,000 less in total services in the year following DBT treatment as compared to the year prior to DBT. In their sample of 41 clients, the total cost decrease was nearly a quarter of a million dollars. Interestingly, the authors also concluded that the cost of providing DBT treatment was not statistically different (actually, about $400 less) than the average outpatient costs from the year before DBT.
Cost effectiveness studies in other countries are difficult to accurately compare with the U.S. due to fluctuations in currency exchange rates, compounding inflation, and vastly different costs in healthcare. However, similar results were reproduced in Australia where a 6-month DBT program reduced number of hospital days by 70% (Prendergast & McCausland, 2007). Another Australian (Pasieczny & Connor, 2011) study found that DBT reduced costs about 33% compared to treatment-as-usual over 6 months. Strikingly, those receiving treatment-as-usual incurred six times more costs due to inpatient bed days. Similar results were reproduced in Sweden (Perseius et al., 2004) and Wales (Amner, 2012).
Alternatively, in attempting to examine benefit instead of cost a Washington State, juvenile offender institution estimated that a $38.05 financial benefit was achieved for every dollar spent on their DBT program (Aos et al., 2004). Similarly, a study in the United Kingdom found that for every 36GBP spent on DBT a 1% reduction in self-harm was achieved (Priebe, 2012). When examining the overall societal cost (based on resource consumption and productivity lose), a German study calculated a nearly 50% reduction in societal cost-of-illness when comparing the treatment year and the year following treatment (Wagner et al., 2014). In summary, economic evaluations of DBT indicate the following: a) reduction in costs when compared to the prior treatment year; b) reduction in costs when compared to treatment-as-usual; c) decrease in long-term service utilization in high service-utilizing individuals; d) a potential financial benefit to the treatment institution and; e) a potential decrease in societal costs.
Citations
American Psychiatric Association (1998). Gold Award: Integrating dialectical behavior therapy into a community mental health program. Psychiatric Services, 49(10). 1338–1340.
Amner, K. (2012), The Effect of DBT Provision in Reducing the Cost of Adults Displaying the Symptoms of BPD. British Journal of Psychotherapy, 28: 336–352. doi:10.1111/j.1752-0118.2012.01286.x
Aos, S.., Lieb, R., Mayfield, J., Miller, M., & Pennucci, A. (2004). Benefits and costs of prevention and early intervention programs for youth. Olympia: Washington State Institute for Public Policy, available at http://www.wsipp.wa.gov/rptfiles/04-07-3901.pdf
Meyers, L. L., Landes, S. J., & Thuras, P. (2014). Veterans’ service utilization and associated costs following participation in dialectical behavior therapy: a preliminary investigation. Military Medicine, 179(11), 1368-1373.
Pasieczny, N., & Connor, J. (2011). The effectiveness of dialectical behaviour therapy in routine public mental health settings: an Australian controlled trial. Behaviour Research andTtherapy, 49(1), 4-10.
Prendergast, N., & McCausland, J. (2007). Dialectic behaviour therapy: a 12-month collaborative program in a local community setting. Behaviour Change, 24(01), 25-35.
Perseius, K-I., Samuelsson, M., Andersson, E., Berndtsson, T., Götmark, H., …. Zinkler, M. (2004). Does dialectical behavioural therapy reduce treatment costs for patients with borderline personality disorder. A pilot study. Vårdi Norden, 24, 27-30.
Priebe, S., Bhatti, N., Barnicot, K., Bremner, S., Gaglia, A., Katsakou, C., & … Zinkler, M. (2012). Effectiveness and cost-effectiveness of dialectical behaviour therapy for self-harming patients with personality disorder: A pragmatic randomised controlled trial. Psychotherapy And Psychosomatics, 81(6), 356-365. doi:10.1159/000338897
Wagner, T., Fydrich, T., Stiglmayr, C., Marschall, P., Salize, H. J., Renneberg, B., … & Roepke, S. (2014). Societal cost-of-illness in patients with borderline personality disorder one year before, during and after dialectical behavior therapy in routine outpatient care. Behaviour Research and Therapy, 61, 12-22.
41 Pdf Previewdialectical Behavioral Training Techniques
Wunsch, E.-M., Kliem, S., Kröger, C. (2014). Population-based cost–offset estimation for the treatment of borderline personality disorder: Projected costs in a currently running, ideal health system, Behaviour Research and Therapy, 60, 1-7
